Hemophilia and genetics
Hemophilia occurs when one of the clotting factor proteins needed for the blood to form clots is missing or reduced. There are at least 13 different proteins — referred to as clotting factors — in the blood that work together to create a fibrin clot when an injury occurs. Clotting proteins are usually designated by Roman numerals (I, II, III, IV, and so on). People who are missing, or have a low amount of, factor VIII (eight) have hemophilia A, the most common type of hemophilia (with von Willebrand Disease being the most common bleeding disorder). It affects about 80 percent of people with hemophilia. People who are missing, or have a low amount of, factor IX (nine) have hemophilia B. Hemophilia B affects about 20 percent of individuals with hemophilia. The incidence (number of new cases) of hemophilia A is approximately 1 in 5,000 males born in the United States.1 The prevalence (number of existing cases) of hemophilia A is about 16,000 people in the U.S. Hemophilia B affects more than 4,100 individuals.2 All races and socioeconomic groups are equally affected.
Acquired hemophilia is a rare autoimmune disorder that can occur in males or females who have other disease states such as rheumatoid arthritis or cancer. It occurs when the person’s immune system reacts by eliminating clotting factor that the patient’s body normally makes. Symptoms are very dramatic, and people who develop it can have extensive visible bruising as well as other bleeding. Treatment revolves around stopping the bleeding symptoms and suppressing the patient’s immune system.
While there are other forms of bleeding disorders like factor XIII (thirteen) deficiency and afibrinogenemia, here you’ll find in-depth information on two of the more frequently occurring factor deficiencies of factor VIII and factor IX.
Clotting factor
Hemophilia has different levels of severity. The amount of factor in the blood will determine the severity level. Severity levels do not change over time in a person with hemophilia.
The level of clotting factor in the blood is linked to the degree of symptoms and determines how severe the condition3 . This is why the level of clotting factor in the blood will determine the severity level.
Classification of Severity of Factor Deficiency3
| Classification | Factor VIII or factor IX level (compared to normal levels) | What to expect |
|---|---|---|
| Severe | Less than 1% | Bleeding after an injury, major trauma, or surgery. May have bleeding without a known injury (spontaneous bleeding). |
| Moderate | 1% to 5% | Bleeding after minor injury is possible and after major trauma or surgery. Occasionally spontaneous bleeding may occur and can be associated with prolonged or serious bleeding in a joint. |
| Mild | 5% to 40% | Prolonged bleeding usually only after serious injury, major trauma, or surgery. |
| Normal | 50% to 150% | No abnormal bleeding. |
How did this happen
Hemophilia is passed on from parent-to-child as an inherited, or genetic, trait. About 30 percent of individuals with hemophilia have no family history of a bleeding disorder and develop hemophilia from a new, spontaneous genetic mutation.4
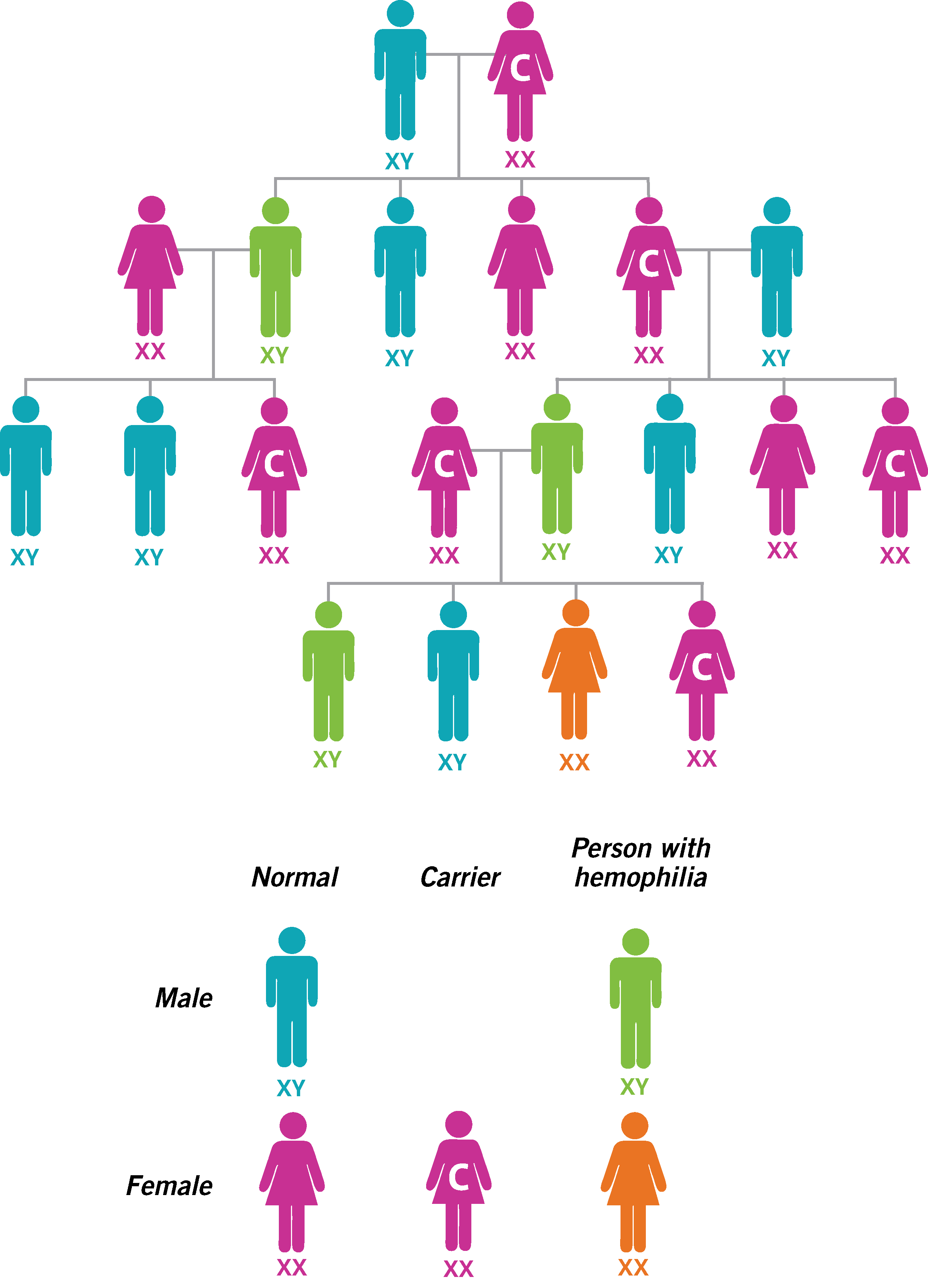
Congenital hemophilia used to be called “the royal disease” since Queen Victoria of England was a hemophilia carrier. A review of her family tree shows how hemophilia was passed through the female descendants, but the symptoms of the disease occurred in the males. How does that happen?
The genes for both hemophilia A and hemophilia B are carried on the X chromosome. Women have two X chromosomes, and men have an X and a Y chromosome. A woman gets pregnant when her egg is fertilized by the man’s sperm. The sperm will carry half of the genetic makeup from the father (including either an X or a Y sex chromosome).
The mother’s egg will carry half of the mother’s genetic makeup and will have an X chromosome. If the father’s X chromosome fertilizes the egg, the baby will be a girl (XX). If the father’s Y chromosome fertilizes the egg, the baby will be a boy (XY). Both hemophilia A and B are X-linked recessive gene disorders. This means that either a single X must be present to have the disorder (in a boy) or girls who are carriers of one X chromosome with a hemophilia gene may have bleeding symptoms. Symptoms in these girls are generally milder than the boys in her family, because her other X chromosome does not have the gene. This is why hemophilia is very rare in females, but many times is passed down from the mother to her son(s).
For a woman who carries the gene for hemophilia, each pregnancy has four possible outcomes: a boy with hemophilia, a boy without hemophilia, a girl who is a carrier, or a girl who is not a carrier. Some carriers can have low levels of clotting factor. They are sometimes called “symptomatic carriers.”
If a man has hemophilia, his daughters will be carriers and his sons will not have hemophilia, since a man does not pass along any X chromosomes to his son(s). Your hematologist will be able to help you better understand this information. A genetic counselor can also help you learn your probability of having a child with hemophilia.
Why does an individual with hemophilia bleed5
Nature has given our bodies the ability to stop bleeding at an injury site. There are three major steps in this process:
- The blood vessel around the area of injury will constrict or become smaller to slow down the amount of blood flowing past the injury.
- Platelets, which are part of our blood, travel to the injury and lay themselves down over the opening. These platelets stick to each other, forming a “platelet plug,” which initially helps stop bleeding.
- Proteins (clotting factors) in the blood create a substance called fibrin, which weaves through the platelets covering the injury and holds the platelet plug in place. This fibrin clot stops the bleeding until the blood vessel can repair itself.
In hemophilia, because one of the proteins (clotting factors) is reduced or missing, not enough fibrin is produced to form the clot. Without the fibrin to weave through the platelets and hold them in place, the platelets wash off the injured area, and the person continues to bleed or starts bleeding again after it initially stops.
Formation of inhibitors6
The immune system is the defense system that normally protects us from illnesses and microscopic invaders like bacteria and viruses that can harm our health. As we are exposed to viruses, the body recognizes the illness and creates antibodies to fight against the illness and rid it from the body. Sometimes the immune system does too good of a job trying to protect us. If the body recognizes factor as a foreign invader, then it can create antibodies against factor. These antibodies neutralize factor and make it ineffective for clotting or cause an allergic-type reaction. This is why people with inhibitors may need to infuse much more factor to overcome the body’s immune response or infuse different products to go around the immune response. About 30% of people with hemophilia A will develop an inhibitor while about 2%-3% of people with hemophilia B will have an inhibitor. If you develop an inhibitor, you and your hematologist will decide how your treatment regimen needs to change.
- 1National Hemophilia Foundation. Hemophilia A. hemophilia.org/Bleeding-Disorders/Types-oaf-Bleeding- Disorders/Hemophilia-A. Accessed Dec. 15, 2016.
- 2Centers for Disease Control and Prevention. Summary Report of UDC Activity. Report date Dec. 31, 2011. https://www.cdc.gov/ncbddd/hemophilia/ Accessed Dec. 19, 2016.
- 3Srivastava A, Brewer AK, Mauser EP et al. Guidelines for the management of hemophilia. Haemophilia 2012:1-47.
- 4National Heart, Lung and Blood Institute. What is hemophilia? nhlbi.nih.gov/health/health-topics/topics/hemophilia. Accessed Aug. 4, 2017.
- 5Banks D. "Introduction to Bleeding Disorders." Nurses' Guide to Bleeding Disorders. National Hemophilia Foundation. 2012.
- 6National Hemophilia Foundation. Inhibitors & Other Complications. hemophilia.org/Bleeding-Disorders/Inhibitors-Other-Complications. Accessed Aug. 18, 2017.